Once the patient reported
that they have all the symptoms, they then will be referred to a Cardiologist
for further checkup and diagnosis to determine that if they suffer from
arrhythmia. The patient will undergo series of diagnosing process such as:
Blood Test
 |
| figure 1. Blood is drawn from a patient |
Blood will be drawn from
their vein and sent to lab to check the level of substances in the blood such
as potassium. Potassium is an electrolyte that sends electrical impulses in the
heart for them to beat and pump the blood throughout the body (University of
Maryland Medical Center, 2015). High level of potassium increases the chances
of getting an arrhythmia because it sends excessive electrical impulses
(Nhs.uk, 2015).
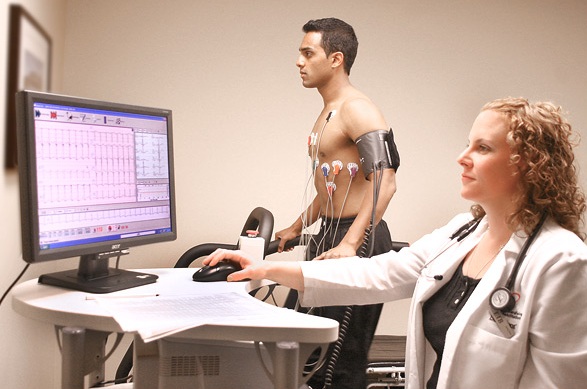
Electrocardiogram (ECG)
 |
| figure 2. Patient undergoing ECG |
This is a standard
cardiology tool for recording heartbeats and its rhythm. It uses electrodes
that act as a sensor to detect the electrical activity of the heart. These
electrodes are attached to certain parts of the chest. Patterns seen on the ECG
could tell if there is a presence of arrhythmia through the irregular waves
that the heart created (Heartrhythmcharity.org.uk, 2015).
Holter Monitor
| figure 3. Holter Monitor with ECG reading |
This is a portable ECG
device that the patient attaches to their chest and it records the patient’s
heart rhythm as they go through their daily routine. They are asked to wear
this device for a day or more to see if they need to undergo more tests before
the cardiologist finally could determine what kind of treatment or medication
that they need (Heart.org, 2015).
Event Monitor
 |
| figure 4. An event monitor placed on patient |
This portable device has
a similar function like a Holter Monitor, but the only difference is that the
patient will be asked to press a button on this device if they experience
arrhythmic symptoms so the cardiologist could check the heart rhythm at the
time of the symptom occurred (Bcpa.co.uk, 2015).
Echocardiogram
 |
| figure 6. Patient being diagnosed |
This is another type of
cardiology tool. It is a noninvasive test that uses sound waves to produce
images of the patient’s heart’s size, structure and motion by placing a
transducer, a hand-held device on the chest (Mayoclinic.org,
2015).
Ambulatory
Electrocardiogram
This device has a
similar function as the Holter Monitor, where it tracks the heartbeat of the
patient but it is used only for 24 hours (WebMD.com, 2015)
If the arrhythmia did
not show up during those tests, the cardiologist will try to trigger the
arrhythmia using as follows:
Stress Test
 |
| figure 7. Patient being assessed |
During a stress test,
the patient will be asked to run on a treadmill or ride a stationary bicycle as
their heart activity is being monitored. The cardiologist may use a drug
instead to stimulate the heart in a way that is similar to exercise if the
cardiologist found out that the patient’s coronary artery disease caused the
arrhythmia, and they appeared to have a difficulty in exercising, (Nhs.uk,
2015).
Tilt Table Test
 |
| figure 8. Process of Tilt Table Test |
This type of test is
only used if the patient had a near fainting spell. The patient will be laid
flat on a table as their heart rate and blood pressure are being monitored.
Along the way, the table will be tilted to a standing position. The cardiologist
will observe how their heart and nervous system respond to the change in angle
(Nhs.uk, 2015).
Electrophysiological
Testing And Mapping.
| figure 9. Placement of Catheter in the heart |
 |
| figure 10. Electrophysiological test and Mapping in process |
In this test, the
cardiologist will insert a thin thread, flexible tubes called catheter that are
tipped with electrodes through the patient’s blood vessels that are connected
to variety spots in their heart. The electrodes are used to map the spread of
electrical impulses throughout the patient’s heart. The cardiologist may also
use the electrodes to stimulate the patient’s heart to beat at rates that may trigger or halt
an arrhythmia. This enables the cardiologist to see the location of the
arrhythmia and determine what may be causing it (Nhs.uk, 2015).



0 comments:
Post a Comment